Diabetic retinopathy is a progressive eye disease that can cause blindness if not treated early.
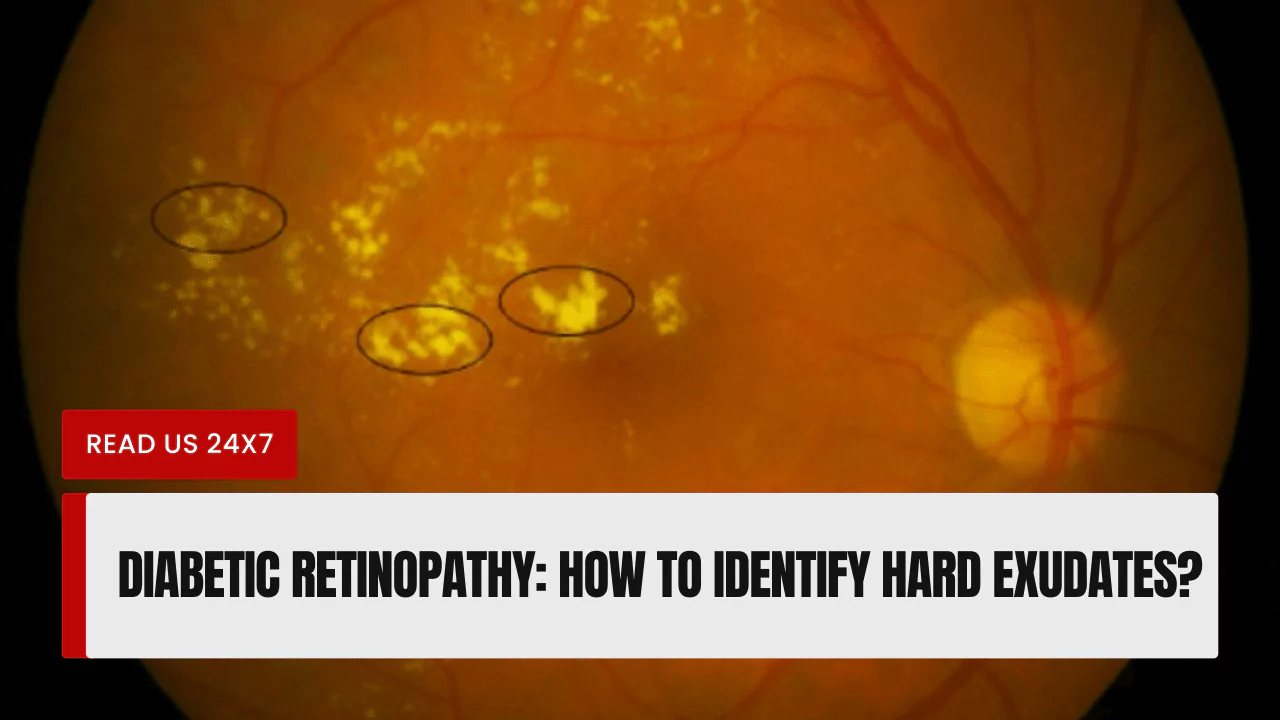
It is the most common cause of blindness in working-age adults. Hard exudates are yellow or white deposits that form on the retina, the light-sensitive tissue at the back of the eye.
They are a sign of diabetic retinopathy and can lead to vision loss if they accumulate in the center of the retina, where the macula is located.
Understanding Diabetic Retinopathy
Definition and Symptoms
Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina. It is caused by high blood sugar levels damaging the blood vessels, making them leak fluid and blood. This can lead to a variety of problems, including hard exudates, macular edema (swelling of the macula), and neovascularization (growth of new blood vessels).
The early stages of diabetic retinopathy often have no symptoms. However, as the disease progresses, people may experience blurred vision, floaters (dark spots or lines in the field of vision), and difficulty seeing at night.
Risk Factors
The risk of developing diabetic retinopathy increases with the duration of diabetes and the level of blood sugar control. Other risk factors include:
- High blood pressure
- High cholesterol
- Pregnancy
- Kidney disease
- Smoking
Pathophysiology
The exact pathophysiology of diabetic retinopathy is not fully understood, but it is thought to be caused by a combination of factors, including:
- High blood sugar levels damage the blood vessels in the retina
- Inflammation
- Increased production of vascular endothelial growth factor (VEGF), a protein that stimulates the growth of new blood vessels
Epidemiology
Diabetic retinopathy causes most working-age blindness in industrialized countries. About 46 million of the 285 million persons with diabetes have diabetic retinopathy.
Diabetic Retinopathy Features and Complications
Hard Exudates
Hard exudates are yellow or white deposits that form on the retina. They are made up of cholesterol, fat, and protein that have leaked out of the damaged blood vessels. Hard exudates are typically harmless, but if they accumulate in the center of the retina, they can cause vision loss.
Macular Edema
Macular edema is swelling of the macula, the central part of the retina that is responsible for sharp central vision. Macular edema can be caused by diabetic retinopathy, but it can also be caused by other conditions, such as age-related macular degeneration.
Neovascularization
Neovascularization is the growth of new blood vessels. It is a common complication of diabetic retinopathy and can lead to bleeding and scarring of the retina.
Management and Treatment Options
The goal of treatment for diabetic retinopathy is to prevent vision loss. Treatment options include:
- Blood sugar control: Good blood sugar control is the most important thing people with diabetes can do to prevent diabetic retinopathy and other complications.
- Blood pressure control: High blood pressure can damage the blood vessels in the retina, so it is important to keep blood pressure under control.
- Laser treatment: Laser treatment can be used to seal off leaking blood vessels and reduce swelling of the macula.
- Injections: Injections of anti-VEGF medications can be used to slow the growth of new blood vessels and reduce swelling of the macula.
- Surgery: Surgery may be necessary in some cases to remove scar tissue from the retina or to repair damaged blood vessels.
How to Identify Hard Exudates?
Hard exudates are typically visible on a dilated eye exam. During a dilated eye exam, the doctor uses eye drops to widen the pupil so that they can get a better view of the retina. Hard exudates may also be visible on optical coherence tomography (OCT), a type of imaging test that creates cross-sectional images of the retina.
Patient Education and Resources for Diabetic Retinopathy
Symptoms to Look Out For
People with diabetes should be aware of the symptoms of diabetic retinopathy, including:
- Blurred vision
- Floaters
- Difficulty seeing at night
- Loss of central vision
Recommended Screening Intervals
People with diabetes should have a comprehensive eye exam at least once a year, even if they have no symptoms of diabetic retinopathy. If they have diabetic retinopathy, they may need to have more frequent eye exams.
Available Medical Options
There are a variety of medical options available to treat diabetic retinopathy, including blood sugar control, blood pressure control, laser treatment, injections, and surgery.